Histoplasmosis is an infection caused by the fungus Histoplasma capsulatum. It usually affects the lungs but can infect other body parts in severe cases. It can occur in people with healthy and suppressed immune systems.
In people with healthy immune systems (including people living with HIV), it may not cause any symptoms, although some people have flu-like symptoms or mild respiratory problems. In people with suppressed immune systems, it can be more serious, including respiratory distress, kidney and liver failure, and brain damage.
Histoplasma is found mostly in the central and eastern United States—especially in the Mississippi and Ohio River areas—and in the Caribbean and South America. It’s most often found in dirt in areas with bird or bat droppings. It is not contagious from person to person.
People can become infected when they breathe in soil or dust contaminated with the fungus. People with HIV who have CD4 counts below 150 are at higher risk of developing histoplasmosis. Although histoplasmosis is an AIDS-defining conditions, it is not a common disease among people living with AIDS, likely due to the use of potent HIV treatment.
What are the symptoms and how is it diagnosed?
The infection often begins and stays in the lungs. At this stage it is called acute disease. If the infection continues there over time, it is called chronic disease. If the infection spreads to other parts of the body, it is called disseminated disease. People can also be infected but not develop symptoms until years later when their immune systems weaken.
Most people who are infected do not experience symptoms, and usually recover without the need for treatment. If symptoms are present, they can include fever, tiredness, weight loss, difficult breathing, chest pain, dry cough, headache, anemia, and enlargement of the liver, spleen and lymph nodes. More symptoms are possible the more the disease spreads.
The higher the CD4 cell count, the more likely it is that histoplasmosis will only involve the lungs. Lower CD4 counts mean that histoplasmosis can move more easily to other parts of the body, including the central nervous system (meningitis). In rare instances, people can experience shock and multiple organ failure.
Your doctor will order a blood and/or urine test to diagnose this infection for acute lung or disseminated disease. A sputum (phlegm) sample from the lungs may also be done, as well as collecting tissue from bone marrow or cerebral spinal fluid if histoplasmosis is suspected in those body parts.
How is it treated?
Treatment depends on the severity of disease. People with healthy immune systems (CD4 counts above 300) don’t usually require treatment for acute lung disease, as the symptoms are usually mild and clear up on their own.
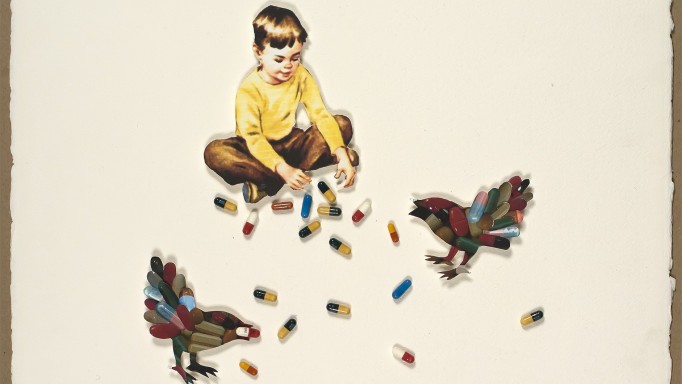
In people with less severe disease, oral itraconazole (Sporanox) is started (not in women in the first trimester of pregnancy) at 200 mg three times a day for three days followed by 200 mg twice a day until symptoms resolve. The liquid form of itraconazole is preferred because it is taken without food and better absorbed by the body, although it has more side effects than the pill form.
In people with moderate to severe disease, liposomal amphotericin B (Ambisome, Abelcet, Amphotec) is given every day through an IV line. Treatment is continued for at least two weeks or until the person is feeling better. Afterwards, daily itraconazole is given up to a year.
If the patient has meningitis, the dose of IV liposomal amphotericin B is usually increased and continued for 4–6 weeks. It is followed by daily intraconazole for at least a year.
After histoplasmosis is successfully treated, liposomal amphotericin B is stopped and intraconazole is started or continued. This is necessary to help prevent histoplasmosis from recurring.
Can it be prevented?
Because the fungus can be found in dirt and soil, it is very difficult to prevent coming into contact with it. Moreover, the fungus can live in a person’s body for many months or possibly years before it causes disease, depending on the health of the immune system.
If your CD4 cell count is below 150, take care when engaging in certain activities—or avoid them altogether—if you live where the fungus is prevalent. It’s a good idea to wear a mouth and nose guard or mask if you garden or work with or disturb surface soil; clean chicken coops; clean, remodel or demolish old buildings; disturb soil with bird or bat droppings; or explore caves.
For people with a CD4 count below 150, taking a preventive medicine is also possible for those at high risk for infection because of their work, activities or residence in a high-prevalence area. Itraconazole is usually prescribed for this and can be stopped when the CD4 count stays above 150 for at least six months.
Finally, an effective way to prevent histoplasmosis is by starting or staying on potent HIV treatment. This helps the immune system prevent the disease from occurring. IRIS (immune reconstitution inflammatory syndrome) has not been reported with histoplasmosis—a condition that causes increased symptoms of an opportunistic infection to happen due to starting or switching HIV treatment.
Are there any experimental treatments?
If clinical trials for HIV-positive patients with histoplasmosis are being conducted, they will most likely be listed on ClinicalTrials.gov, a site run by the U.S. National Institutes of Health. The site has information about all HIV-related clinical studies in the United States. For more info, you can call their toll-free number at 1-800-HIV-0440 (1-800-448-0440) or email contactus@aidsinfo.nih.gov.
Last Reviewed: January 24, 2019