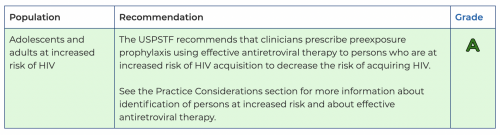
The U.S. Preventive Services Task Force (Task Force) [on August 22] published a final recommendation statement on pre-exposure prophylaxis (PrEP) for the prevention of HIV. Based on its review of the evidence, the Task Force recommends that healthcare professionals prescribe PrEP to people at increased risk for HIV to help prevent HIV. This is an A grade.
USPSTF
HIV is a virus that attacks the body’s immune system. While it can be treated, HIV is not curable and can have significant health consequences, making prevention very important. PrEP is a safe, highly effective way to help prevent HIV in people who do not have HIV but are at increased risk of getting it. There are now three FDA-approved PrEP medications in the United States—two are pills, and one is a shot. PrEP is most effective when taken as prescribed. The Task Force encourages healthcare professionals to help their patients who are on PrEP understand the importance of taking it as prescribed and support them in doing so.
“PrEP is an essential tool to help reduce rates of HIV in our nation,” says Task Force member John B. Wong, MD. “To prevent HIV, it’s important that healthcare professionals prescribe PrEP to patients at increased risk and discuss which form of this medication would be best for them.”
PrEP is only for people who are at increased risk for HIV. To determine risk, healthcare professionals need to talk with all their patients about their sexual history and ask about injection drug activities in an open and supportive way. Factors that increase a person’s risk for HIV include having sex with someone who has HIV; having a recent sexually transmitted infection (STI); not using condoms consistently, especially with partners who are at increased risk; and sharing drug injection needles.
Black and Hispanic/Latino people are more likely to be diagnosed with HIV yet have much lower rates of PrEP use than White people. Healthcare professionals need to be aware that barriers to PrEP use exist and provide support to patients at increased risk in these communities to start and stay on PrEP. The Task Force is calling for more research on how to reduce barriers in communities most impacted by HIV.
“We’re still seeing that many people who could benefit from PrEP aren’t receiving this highly effective medication, particularly in Black, Hispanic, and Latino communities,” says Task Force member James Stevermer, MD, MSPH. “It’s critical for healthcare professionals to keep these disparities in mind and to have conversations with patients who are at risk about proven ways to prevent HIV, including taking PrEP.”
It is important that people who take PrEP use condoms consistently, practice other safer sex behaviors, and receive ongoing care, including testing for HIV and other STIs.
The Task Force’s final recommendation statement and corresponding evidence summary have been published online in the Journal of the American Medical Association, as well as on the Task Force website at: https://www.uspreventiveservicestaskforce.org. A draft version of the recommendation statement and evidence review were available for public comment from December 13, 2022, through January 17, 2023.
The Task Force is an independent, volunteer panel of national experts in prevention and evidence-based medicine that works to improve the health of people nationwide by making evidence-based recommendations about clinical preventive services such as screenings, counseling services, and preventive medications.
Dr. Wong is vice chair for Academic Affairs, chief of the Division of Clinical Decision Making, and a primary care clinician in the Department of Medicine at Tufts Medical Center. He is also a professor of medicine at Tufts University School of Medicine.
Dr. Stevermer is the vice chair for clinical affairs and Paul Revare, MD, professor of family and community medicine at the University of Missouri (MU). He is the medical director of MU Health Care Family Medicine–Callaway Physicians, where he practices and teaches rural primary care. His scholarly activities focus on dissemination and evidence-based medicine.
This blog post was published by HIV.gov on August 23, 2023. It was cross-posted from the USPSTF News.








Comments
Comments